The microbial world is engaged in a silent, invisible war—one that has raged for billions of years and now threatens to undermine modern medicine. At the heart of this conflict lies the relentless evolution of antibiotic resistance, a phenomenon that transforms harmless bacteria into formidable adversaries. Scientists are racing to understand this evolutionary arms race, peering into petri dishes and sequencing genomes to decode the strategies microbes employ to outmaneuver our most potent drugs.
In laboratories around the globe, researchers observe something extraordinary: bacterial colonies exposed to antibiotics don’t simply perish. Instead, they adapt with startling ingenuity. Some deploy molecular pumps to eject drugs from their cells, while others produce enzymes that dismantle antibiotics before they can take effect. The most alarming adaptations involve horizontal gene transfer—bacteria swapping resistance genes like soldiers passing ammunition in a battlefield. These mechanisms aren’t theoretical; they’re happening right now in hospitals, farms, and even the human gut.
The story of antibiotic resistance isn’t new. Alexander Fleming himself warned of it when he discovered penicillin in 1928. But the scale has escalated dramatically. Overprescription in human medicine, rampant use in livestock, and improper disposal of pharmaceuticals have turned every environment into a training ground for resistant strains. A 2019 UN report estimated that drug-resistant infections could claim 10 million lives annually by 2050 if unchecked—a statistic that hangs over the medical community like a specter.
Evolutionary biologists have uncovered an unsettling pattern: resistance often emerges long before humans deploy an antibiotic. Soil-dwelling bacteria, locked in their own chemical warfare for eons, already possess resistance genes to most clinical antibiotics. When we introduce these drugs into ecosystems, we’re effectively selecting for pre-existing defenses. This revelation has shifted the paradigm—resistance isn’t created by antibiotics; it’s merely amplified by them.
One particularly chilling case involves Mycobacterium tuberculosis. Strains resistant to all known TB drugs have emerged, forcing physicians to resurrect toxic treatments from the 1940s. Similarly, gonorrhea—once easily cured—now has untreatable variants spreading globally. The WHO’s list of "priority pathogens" reads like a most-wanted roster of microbial criminals, each capable of shrugging off multiple drug classes.
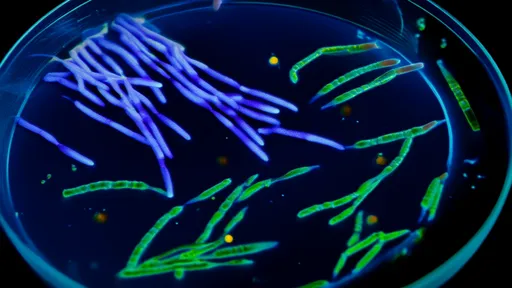
Yet within this crisis lies fascinating science. Researchers at Harvard created a mesmerizing visualization of bacterial evolution—a two-foot-square petri dish with escalating antibiotic concentrations. At the edges, susceptible bacteria halt, but mutants conquer each successive drug-laden ring until they reach the center. This "mega-plate" experiment, shared virally in 2016, became the iconic image of resistance evolution, demonstrating how easily bacteria achieve what would take humans millennia of genetic engineering.
The agricultural sector plays a paradoxical role. While livestock antibiotics accelerate resistance, they’ve also revealed unexpected solutions. Scientists discovered that withholding certain antibiotics actually makes bacteria more vulnerable—a counterintuitive phenomenon called "collateral sensitivity." Some drug combinations create evolutionary traps where resistance to one antibiotic increases susceptibility to another. These insights inspire innovative treatment strategies that could outflank resistant strains.
Phage therapy—using viruses that prey on bacteria—has re-emerged as a promising alternative. In 2019, a teenage cystic fibrosis patient in London received phage treatment against a drug-resistant infection when all else failed. Within weeks, her life-threatening condition improved dramatically. While phages aren’t a silver bullet (they’re highly specific and can trigger immune responses), they represent the kind of creative thinking the post-antibiotic era demands.
Perhaps the most profound realization is that we’re not just fighting bacteria—we’re battling evolution itself. Microbial generations pass in minutes, allowing evolutionary experiments that would take mammals centuries. This speed, combined with vast population sizes and genetic promiscuity, makes resistance inevitable. The question isn’t whether resistance will emerge, but how we can stay ahead of it.
Policy changes are gaining momentum. Sweden’s 1986 ban on antibiotic growth promoters in livestock didn’t harm productivity as feared—instead, it reduced resistance rates. The Netherlands followed suit, cutting veterinary antibiotic use by 70% since 2009. Meanwhile, diagnostic advancements like rapid resistance testing could help tailor treatments and reduce unnecessary prescriptions.
On the innovation front, CRISPR gene-editing offers tantalizing possibilities. Some labs are designing "gene drives" to spread susceptibility genes through bacterial populations, essentially reversing resistance. Others explore antimicrobial peptides from unlikely sources—frog skin, scorpion venom, even platypus milk. These unconventional approaches highlight how much we still have to learn from nature’s chemical arsenal.
The economic dimension can’t be ignored. Developing new antibiotics is financially unattractive for pharmaceutical companies—drugs are used briefly and lose efficacy over time. Creative incentives like subscription-based payment models (where governments pay for access rather than volume) aim to reinvigorate the pipeline. The PASTEUR Act proposed in the U.S. Congress exemplifies this shift in thinking.
Public awareness remains shockingly low. A 2020 survey found that 65% of Europeans believe antibiotics kill viruses—a dangerous misconception fueling misuse. Educational campaigns targeting schools, pharmacies, and social media could help, but must compete with vaccine misinformation and general science skepticism. Changing behavior requires making the invisible visible—helping people understand that every unnecessary antibiotic prescription contributes to a global threat.
Looking ahead, the solution likely lies in integration—combining new drugs with phage therapy, immunotherapies, and good old-fashioned infection control. Hospitals reducing MRSA through rigorous hygiene protocols prove that low-tech measures remain essential. The "One Health" approach—recognizing connections between human, animal, and environmental health—is gaining traction as the only viable framework.
The antibiotic era may be entering its twilight, but the story isn’t over. From AI-discovered molecules to fecal transplants that restore healthy microbiomes, science continues its duel with evolution. What’s clear is that arrogance is our greatest vulnerability—assuming technological superiority over organisms that have survived every extinction event. The microbes aren’t evolving; they’re reminding us how evolution works. Our task isn’t to win the war, but to achieve a sustainable stalemate.

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025